We had the honour of providing some pre-ESPYs fixing for the amazing athletes and special guests in attendance because the best deserve the best.
![the[fix]](http://images.squarespace-cdn.com/content/v1/5494e530e4b039edeef75dff/1467052868801-4WDDECP8CV27LAFWPL65/the%5Bfix%5D+logo+TM.jpg?format=300w)
Get fixed

Golf, baseball and tennis are very different sports with diverse game play structures. However, athletes across all three seem to share similar goals: they want to move the ball faster, harder and more accurately than their opponent. They also want to have high consistency for as many repetitions as possible. During each repetition, the athlete transfers force from their legs, through their torso and arm to impact the ball. The elbow acts as a pivot point where rotary torque is converted into linear acceleration to move the ball. High repetition combined with excessive force applied at the elbow makes it prone to injury. The most common elbow injuries in these athletes include Golfers Elbow (AKA Pitchers Elbow or medial epicondylitis), Tennis Elbow (AKA lateral epicondylitis) and nerve injuries involving the radial, median or ulnar nerves.
Golfer’s Elbow (AKA Pitchers Elbow or Medial Epicondylitis):

Golfers elbow is characterized by inflammation of the tendon that connects the forearm flexors and pronator muscles to the inside of the elbow. Many muscles share this common attachment site. Repeated, forceful loading of these muscles causes pain along the inside of the elbow accompanied by weakness in grip strength and wrist flexion. This injury is most common in golfers, throwing athletes, bowlers, archers, tennis players and weight lifters. Conditions that can mimic golfers elbow include cervical radiculopathy, little league elbow and ulnar collateral ligament (UCL) tears.
Little league elbow occurs in children with a similar mechanism of injury. However, since their growth centers are still open, repeated tugging on the attachment can cause a traction fracture. Little league elbow requires immediate medical attention to stabilize the elbow joint and to ensure proper bone development.
Ulnar collateral ligament (UCL) injuries are also very serious and require medical attention. The UCL supports the inside of the elbow and protects the elbow joint against load. Tommy John surgery is the procedure used to stabilize the elbow following a UCL tear.
Tennis elbow (AKA lateral epicondylitis):

Tennis elbow is characterized by the same symptoms, but it is located on the other side of the elbow joint. The extensor and supinator muscles of the forearm share a common tendon that attaches to the outside of the elbow. Overuse and repeated, forceful wrist extension causes inflammation and pain at the elbow. This condition can occur in any occupation that requires repeated wrist extension or prolonged gripping such as plumbers, carpenters and chefs. Tennis elbow is easily identified with palpation along the outside of the elbow and through muscle testing.
The treatment approach for both Golfers and Tennis elbow are almost identical except for where the therapy is applied. Warming up before activity will go a long in preventing these injuries. Start with slow, controlled repetitions and move towards full speed motions in a graded fashion. In acute situations, RICE principles (rest, ice, compression and elevation) and activity modification are important. Anti-inflammatory interventions such as applying ice, taking fish oil supplements and NSAID’s may be appropriate.
Physical therapy is an essential component of care. Treatment will focus on maintaining range of motion, improving strength, bracing the joint and reducing pain. This will include a combination of acupuncture, soft tissue massage, stretching, mobilization, taping and strengthening exercises.
Nerve Entrapment at the Elbow (medial, radial, ulnar):
The main nerves that supply your arms include the radial, ulnar and median nerves. As we move, the nerves are stretched and compressed as they travel through tight spaces. Each nerve can become irritated as specific locations around the elbow. The most common compression sites include:

1) Pronator Teres Syndrome: The median nerve is compressed by the pronator teres muscle located in the front of the forearm. This can cause forearm weakness and/or numbness in the thumb and first two fingers and weak grip strength. This condition can be confused with carpel tunnel syndrome if not properly assessed.
2) Cubital Tunnel Syndrome: The ulnar nerve is compressed within the cubital tunnel located behind the inside of the elbow. At the elbow, the ulnar nerve travels close to the skin and is not protected by bone. If an external force hits the nerve, it causes a shooting pain towards the arm known as hitting your “funny bone.” This condition can cause numbness or tingling into the 4th and 5th fingers, grip strength weakness and a claw hand deformity.
3) Supinator Syndrome: The radial nerve is commonly irritated as it passes underneath the supinator muscle in the back of the forearm. This condition causes weakness with wrist extension and numbness in the back of the hand.

The goals for treating peripheral nerve injuries includes maintaining a full range of motion, reducing inflammation, improving mobility of the nerve and reducing pain levels. Treatment includes RICE principles, activity modification, nerve flossing, soft tissue massage, acupuncture, mobilization, splints/taping and muscle strengthening.
The nerve injuries explained above are the most common around the elbow. This does not represent a comprehensive list of possible causes. If you experience any weakness, numbness or tingling in the arms you should have it properly assessed and treated to prevent further deterioration.
References:
Young CC. (2016). Medscape: Medial Epicondylitis. Updated on April 19th, 2016. Retrieved from: http://emedicine.medscape.com/article/97217-overview#a6 on May 8th, 2017.
AAOS. OrthoInfo: Tennis Elbow (Lateral Epicondylitis), American Academy of Orthopedic Surgeons (AAOS). Updated July 2015. Retrieved from: http://orthoinfo.aaos.org/topic.cfm?topic=a00068 on May 9th, 2017.
Neal, S. L., & Fields, K. B. (2010). Peripheral nerve entrapment and injury in the upper extremity. American family physician, 81(2).

Running outdoors is an incredible way to get some fresh air, exercise and squeeze in a well-deserved mental break after a long workday. As spring emerges, many people will dust off their old runners and hit the trails. It is important to start slowly and build up towards your fitness goals. Try not to compare your current performance to your ability at the end of last summer. This will set you up for disappointment. Start slow and each day push a little harder and run a little further. As the old saying goes: ‘it’s a marathon, not a sprint.”
Regardless of your motivations for getting active, you will likely experience fatigue and injury along the way (to varying degrees). Three repetitive running injuries that we commonly treat include patellofemoral pain syndrome (runner’s knee), shin splints and plantar fasciitis. These conditions can be brought on by a sudden increases in training frequency, intensity or duration (“too often, too fast and too much”). Self-management techniques go a long way towards preventing these injuries. Carefully plan your workouts allowing for adequate rest between sessions accompanied by appropriate nutrition. Make sure you stretch before every workout and maintain optimal form while running.

Patellofemoral Pain Syndrome (PFPS):
Patellofemoral pain syndrome (PFPS) accounts for 16-25% of all running injuries. It is described as pain behind, underneath or around the kneecap and is aggravated by running, forceful or repetitive knee extension, squatting or jumping. Sometimes a popping sound, grinding sensation or mild knee buckling can occur. PFPS is a functional diagnosis and is considered after more serious injuries are ruled out. PFPS is associated with three major contributing factors:
a) Malalignment of the lower limb or knee cap (“poor knee tracking”)
b) Muscular imbalance around the knee (especially quadriceps-hamstring strength ratio)
c) Overactivity (eg. increased running/cycling mileage)
A basic principle in physical therapy is to identify the contributing factors of a condition, and to use those to guide treatment. Therefore, treatment for PFPS aims to improve knee tracking, optimize muscle balance around the knee and alter your current activity levels. Activities like squatting, kneeling, cycling with a low seat or excessive running should be avoided. Treatment may include any combination of RICE principles (rest, ice, compression and elevation), strength training, stretching, Kinesiotape or athletic tape, soft tissue therapy, NSAID’s, gait retraining, knee braces and/or prescription orthotics. At the[fix], we use 3D Gaitscan technology to analyze your gait and cast you for custom fit orthotics. Orthotics are covered by most insurance plans.
Shin Splints (Medial Tibial Stress Syndrome):
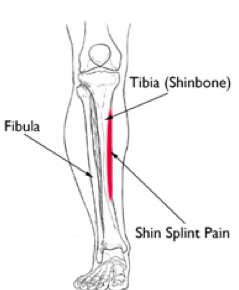
Shin splints produce a vague, diffuse pain along the inside of the shinbone (tibia). Recently, shin splints has become a catch all term to describe any type of shin pain. Tibialis anterior strains get incorrectly grouped in with shin splints even though they occur on the opposite side of the tibia. True shin splints happen on the INSIDE of the tibia rather than the outside.
Repetitive muscle contraction of the tibialis posterior and flexor digitorum pull on their attachment to the tibia causing inflammation and micro-tearing at the bone surface. Having flat feet, high arches and wearing improper footwear can contribute towards this condition. It is important to differentiate shin splints from stress fractures, chronic exertional compartment syndrome and acute tendonitis.
Self-management techniques for this condition include a combination of RICE principles, stretching, strength training, activity modification and ensuring proper footwear. Massage therapy, orthotics, acupuncture, taping and gait pattern analysis can help to relieve pain and improve recovery. At the[fix] we use a tailored combination of these treatment methods to ensure we are addressing your unique injury.

Plantar Fasciitis:
Plantar fasciitis is one of the most common foot complaints in athletic and non-athletic populations. The plantar fascia is a thick band of connective tissue that lines the base of the foot that connects your heel to the base of your toes to support your arches. Plantar fasciitis involves inflammation of the plantar fascia due to repetitive overuse. Pain is felt along the inside arch with focal pain towards the heel.
Poor running shoes and running on an uneven surface promotes the development of plantar fasciitis. Risk factors include prolonged standing, being flat-footed, poor ankle range of motion and heel spurs. Treatment includes a combination of massage therapy, intrinsic foot muscle and calf strengthening, taping, acupuncture and joint mobilization. Custom orthotics, night splints or gait retraining may also be warranted. If severe inflammation is present, then your medical doctor may prescribe anti-inflammatory medications. At the[fix], most of our patients respond well to a conservative treatment approach and are able to return to normal activity in a few months.
Conclusion:
Running is one of the best workouts you can do for overall heath. Make sure you take advantage of the beautiful sunshine because it only lasts a few months! Get outside and get healthy! Take preventative measures to reduce your chance of experiencing these common running injuries. Gradually build up the duration, frequency and intensity of your workouts. Logging your mileage and timing yourself are good ways to keep track of your progress. Make sure you are diligent with stretching and strengthening to prevent fatigue and injury. If you are experiencing any of these symptoms or would like advice, book an appointment today for an Initial Chiropractic Assessment and Treatment. During this visit we may recommend a combination of registered massage therapy, custom orthotics, exercise prescription and/or acupuncture in addition to comprehensive chiropractic treatment.
References:
AAOS. (2012). Otho Info: Shin Splints, The American Academy of Orthopedic Surgeons (AAOS). Updated: May 2012. Retrieved from: http://orthoinfo.aaos.org/topic.cfm?topic=a00407.
Buchbinder, R. (2004). Plantar fasciitis (Clinical Practice), New England Journal of Medicine, 350:2159-2166.
Galbraith, R. M., & Lavallee, M. E. (2009). Medial tibial stress syndrome: conservative treatment options. Current reviews in musculoskeletal medicine, 2(3), 127-133.
Mayo Clinic Staff. (2016). Plantar fasciitis: Patient Care & Health Information, Mayo Clinic. Retrieved from: http://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/home/ovc-20268392.
Moen, M.H., Tol, J.L., Weir, A., Steunebrink, M., De Winter, T.C. (2009). Medial tibial stress syndrome: A critical review, Sports Medicine, 39(7):523-545.
Schiepsis, A.A., Leach, R.E. Gouyca, J. (1991). Plantar fasciitis: etiology, treatment, surgical results and review of the literature, Clinical Orthopaedics & Related Research, 226.
Thomee, R., Augustsson, J., Karlsson, J. (1999). Patellofemoral Pain Syndrome: A Review of Current Issues, Sports Medicine, 28(4):245-262.
This April has been extremely exciting for sports fans in Toronto! The Blue Jays and Toronto F.C. just began their season while the Raptors and Maple Leafs were both in the playoffs for the first time since 2002. The Toronto Wolfpack rugby team will play their first home game in early May making them the only transatlantic professional sports team in history. It is certainly a good time to be a Toronto sports fan!

Not only are professional athletes getting active during the spring, but many of us will join recreational leagues as well. Whether this involves slow pitch baseball, golfing, beach volleyball or training for a marathon, it is important to take care of your body to perform optimally and maximize the longevity of your athletic “career.”
We tend to see a large influx of athletes and weekend warriors seeking therapy for injuries that occur from re-engaging in athletic endeavors. Keep your eyes locked to our blog over the next few months! We will be discussing common athletic injuries that we see every day at the[fix]. We will explain how the injuries occur, what you can do to prevent them and how we treat your injuries in the clinic. If you have a particular injury that you wish to learn about, please comment below, email us or speak with your provider at the [fix]!